Loading...
Corneal problems such as Keratoconus, Fuchs corneal dystrophy, post surgery corneal decompensation and infections can compromise the corneal transparency, leading to progressive scarring and loss of vision. This is termed as corneal blindness. Corneal transplantation is the surgical procedure undertaken to cure corneal blindness. It involves replacement of the patient’s diseased cornea with a healthy cornea obtained from deceased human donors who have kindly donated their eyes for this purpose. The UK eye banks are instrumental in providing donor corneas and undertaking a complete health check prior to transplantation.
Mr Rajan performs corneal transplant procedures routinely at
Addenbrookes Hospital, Cambridge for NHS patients. These
procedures are not routinely available on a private patient basis due
to UK wide corneal transplant shortage

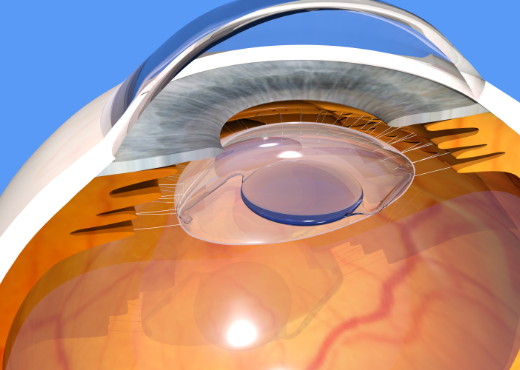


Human cornea is the clear “window” of the eye. It is approximately 0.5mm thick and 12mm across. It lies in front of the fluid filled anterior chamber of the eye and the coloured iris. It is like the lens of a camera - any opacity or distortion results in a poorly focused image. It has 3 layers:
1. The thin surface “skin” (or epithelium)
2. The thick central layer (or stroma) and
3. The single layer of cells on the back surface (or endothelium) – this last layer is made of cells that are not replaced through life (when damaged the place of the dead cells is taken by enlargement and movement of their healthier neighbours. All of these layers must be clear and smooth for the cornea to work as a window. The cells of the back surface layer (endothelium) pump fluid out of the cornea to maintain its thickness at about 0.5mm – if this layer stops functioning normally the corneal thickness increases and when it reaches about 0.6mm it starts to become opaque (corneal failure or decompensation), at about 0.8mm the cornea becomes waterlogged resulting in blistering of the “skin” (bullous keratopathy) leading to pain in addition to blindness.
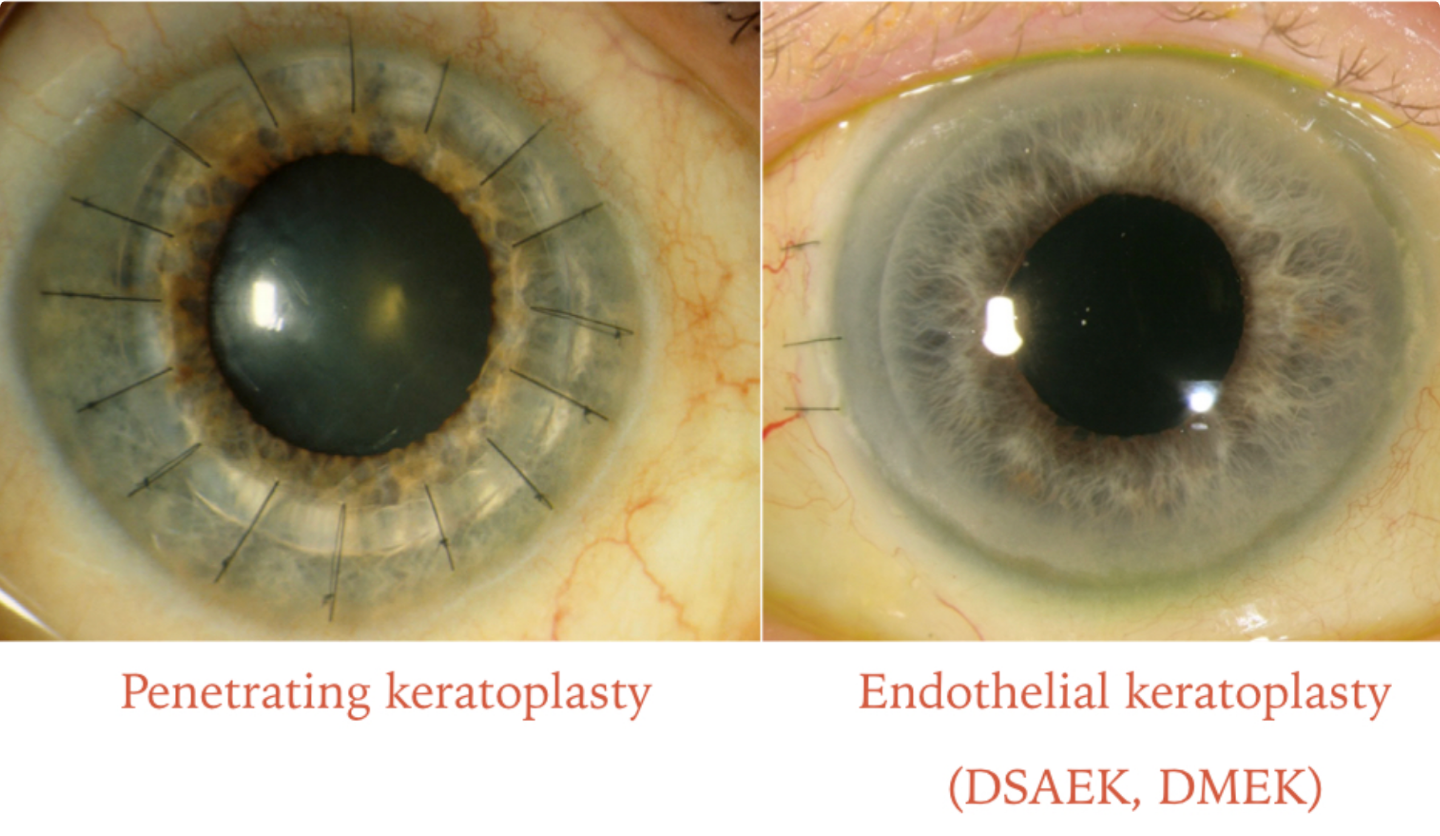
There are two principal types: partial thickness (or lamellar) or full thickness (or penetrating).
Penetrating (full thickness) corneal grafts have been the most widely carried out for all types of corneal disease for 40 years. However this type of graft is only mandatory if there is deep corneal scarring OR when the corneal disease involves both the endothelium AND the stroma . For epithelial and stromal diseases it is carried out because it is easier to replace the whole cornea rather than a layer and because the vision is possibly better after a full graft; the alternative lamellar procedure is the deep anterior lamellar keratoplasty (DALK). The down side of the penetrating graft is the higher risk of transplant rejection, the need for multiple sutures to secure the transplant and delayed visual rehabilitation. In addition, it is difficult to redo a full thickness graft later in life as opposed to a partial thickness corneal transplant. Therefore, for corneal endothelial diseases such as Fuchs dystrophy, penetrating grafts have been superseded by selective lamellar keratoplastytechniques such as DSAEK and DMEK.
Lamellar (partial thickness) corneal grafts are used for reasons outlined below. They may be anterior OR posterior.
Anterior lamellar grafts are widely used because of the benefits of greatly reduced risk of rejection and late graft failure and the development of better techniques for doing the surgery. They are only suitable for use in conditions affecting the front layer (epithelium) and central layer (stroma) of the cornea. The down side is that the technique of deep lamellar keratoplasty is technically difficult and if the endothelium is perforated during the surgery, the surgeon needs to convert to a full (or penetrating) graft during the operation. Also the vision following a successful lamellar graft might not match the vision following a successful penetrating graft, although the differences are small.
Posterior lamellar grafts are a recent innovation. However the results of several thousand patients worldwide have now reported successful outcomes. Technically the posterior lamellar graft is termed Descemet’s stripping automated endothelial keratoplasty (DSAEK) and Descemets membrane endothelial keratoplasty (DMEK).
The benefits of both DSAEK and DMEK are
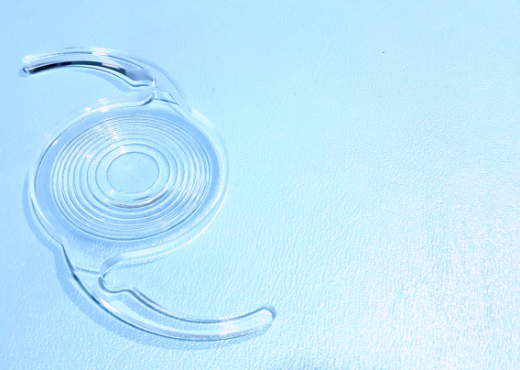
1. It is a small incision technique which is carried out under local anaesthesia through a 5 mm incision, and requires only a few stitches to close the wound.
2. It leaves the eye much stronger than after a penetrating graft and also eliminates the problems of regular and irregular astigmatism that accompany all penetrating grafts.
3. It speeds up the recovery period (3 months compared to 12-18 months with penetrating grafts).
4. It reduces the risk of graft rejection.
The down side is that the attachment of the transplant to the back of the patient’s cornea might not be total. In this case transplants may dislocate in the first 24 hours in up to 10% of cases and might require minor adjustment in the post operative phase. If this happens it is normally possible to reattach the graft with an air injection under local anaesthesia. Posterior lamellar grafts are prone to immune rejection similar to penetrating grafts and therefore patients should not stop taking steroid eye drops for up to 12 months in the least. DSAEK and DMEK can undergo failure due to endothelial loss and it is possible to redo the procedure with repeat DSAEK procedure.
• Patients having DSAEK and DMEK can expect stable vision within 2-4 months after surgery but will still require eye drops for 12 – 24 months or more.
• If you are forgetful about your treatment: you must be able to take eye drops for a minimum of 12 months; forgetting to take medication is a frequent cause of graft failure.
Cambridge Vision Clinic based in Cambridge, UK features an excellent team of eye care professionals offering a personalised, safe approach to patients with cataract and eye disorders for over 10 years.
Email: info@cambridgevisionclinic.org
Phone: 07871660645
Fax: 01223 266 958